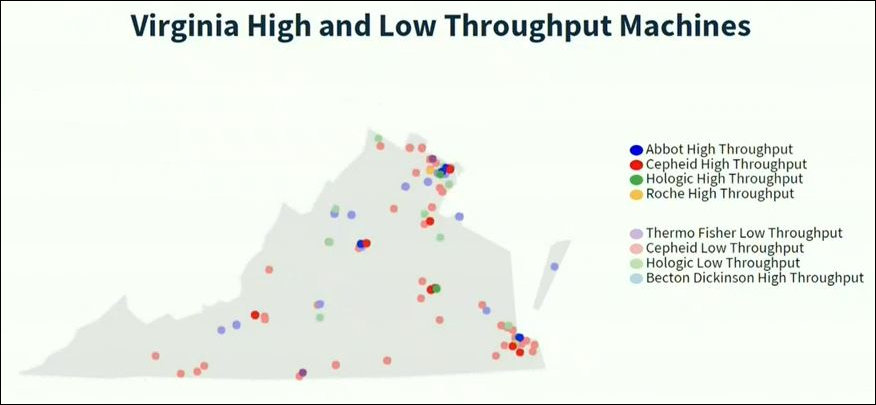
Perhaps this slide will prove useful to the task force just appointed by Governor Ralph Northam to address the disarray in the Virginia Department of Health’s COVID-19 testing program. In the face of a declining number of tests reported to the Virginia Department of Health in the past week, Northam has said he won’t relax emergency measures shutting down Virginia’s economy until the state boosts its capacity to test and measure the incidence of the disease.
The slide, taken from a presentation by Deborah L. Birx, coronavirus response coordinator for the White House, shows the location of dozen high- and low-throughput testing machines across Virginia. Said Birx yesterday:
We wanted every governor and every state and health laboratory director to have a clear understanding of the full capacity within the state – both for the capacity, but also where technical assistance and additional supplies may be available. … Every governor not only received the Excel spreadsheet with the complete list of the equipment and the ZIP Code of the location and the laboratory to really be able to create a mosaic of laboratories of the high-speed and low-speed equipment together to meet the needs of their clients, depending if they’re drive-through or hospital needs. … Continue reading







 By Dick Hall-Sizemore
By Dick Hall-Sizemore