The patient population of the Canterbury Rehabilitation and Healthcare Center, site of nearly 50 COVID-19 deaths, consists primarily of Medicaid recipients. The facility recently changed ownership and was previously known as Lexington Court Rehabilitation and Healthcare Center.
Nursing Home Compare Five-Star Quality Rating System
A nursing home is a place for people who can’t be cared for at home and need 24-hour nursing care. This Medicare 5-star rating system was developed to help individuals, family members, and the public compare the quality of nursing homes more easily by synthesizing a large volume of information on the website into an easily viewable star rating system. CMS based the Overall Ratings on an algorithm that calculates a composite view of nursing homes from three measures: results from approximately three years of onsite inspections carried out by trained surveyors; performance on certain quality measures; and self-reported nursing staffing levels.
Nursing homes provide skilled care to people who can’t be cared for at home and need 24-hour nursing care. Skilled care includes skilled nursing or rehabilitation services to manage, observe, or assess a resident’s care. Examples of skilled care include occupational therapy, wound care, intravenous (IV) therapies, and physical therapy.
CMS creates the overall star rating for nursing homes from 3 parts: (1) Health inspections (2) Quality of resident care measures and (3) Staffing.
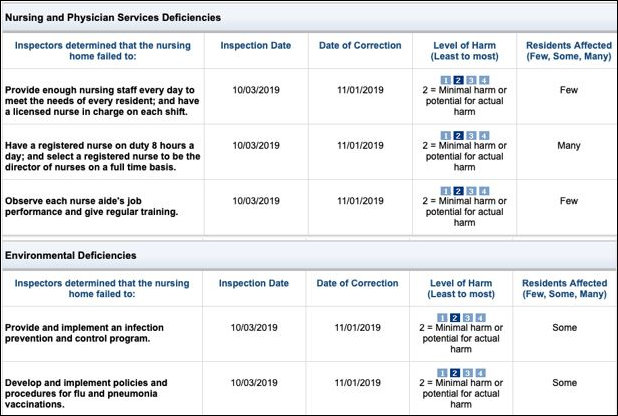
Inspection Data
CMS bases Five-Star quality ratings in the health inspection domain on the relative performance of facilities within a state. From Medicare.gov records, based on an October 3, 2019 inspection, Canterbury was deficient in both staffing and infection control. I reviewed the report of the October 3, 2019, inspection, and it referred to only a single instance of a staffing shortage. The last of entries in the four-page report of the deficiency ID Prefix tag F 0725, “Provide enough nursing staff each day to meet the needs of every resident…” were:
“On 10/3/19 at 4:12 p.m., ASM #3 (Administrative Staff Member) stated the facility did not have a policy regarding staffing.
On 10/3/19 at 4:47 p.m., ASM #1 stated he had no further information regarding the 9/22/19 nursing staff concern.
No further information was presented prior to exit.”
The inspection report recognized three Level 2 staffing deficiencies. Level 2 is defined as:
No actual harm with a potential for more than minimal harm that is not immediate jeopardy: noncompliance with the requirements that results in the potential for no more than minimal physical, mental, and/or psychosocial harm to the residents or employees and/or that result in minimal discomfort to the residents or employees of the facility, but has the potential to result in more than minimal harm that is not immediate jeopardy.
It is hard to reconcile the findings of:
- insufficient nursing staffing;
- the absence of a registered nurse (RN) on duty; and
- the lack of an RN Director of Nursing
in a nursing home full of sick people with an assessment that the absence reflected “minimal harm or potential for actual harm”.
A re-inspection on October 25 did not report these same shortfalls. One is left to assume one of two things: that by the absence of staffing and infection control shortfalls recorded in an October 25 follow-up report or that by a letter of correction submitted by the facility or both those deficiencies were reported as corrected on November 1, 2019 as shown above.
The current health inspection rating of Canterbury Rehabilitation and Health Care Center on the Medicare Nursing Home Compare website is based on the October 3rd inspection. There is no indication on that site that the discrepancies were corrected. We also see that the facility was not self-reporting complaints.
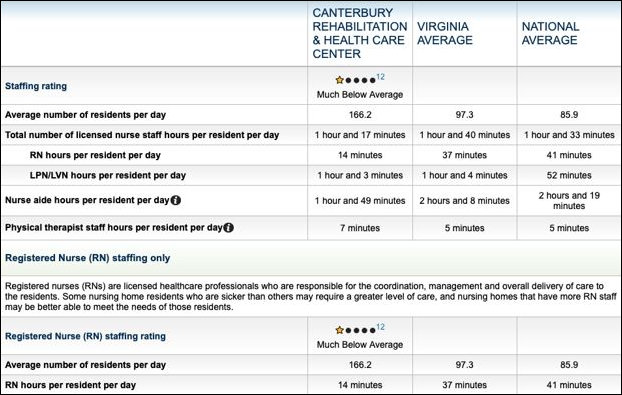
Staffing
Staffing domain data are case-mix adjusted using the Resource Utilization Group (RUG III) categories. Case-mix adjustments allow for a fair comparison of staffing across facilities with different levels of resident acuity. Ratings on the staffing domain for nursing homes are based on two measures: (1) Registered nurse (RN) hours per resident per day; and (2) total nurse staffing (the sum of RN, licensed practical nurse (LPN), and nurse aide) hours per resident per day. In a skilled nursing facility, physical therapist hours are considered also.
For each of RN staffing and total staffing, a 1 to 5 rating is assigned according to thresholds established for each rating category. These ratings are then combined to assign an overall staffing rating.
For example, to get an overall staffing rating of five stars, nursing homes must earn a rating of five stars for both RN and total staffing. Nursing homes also may be assigned a on- star rating if they do not have an RN onsite every day, do not submit staffing data, or their data cannot be verified.
Nursing Home Compare data and the records of vhi.org each were last updated March 31, 2020. In the March 31 data, 42 of Virginia’s 286 Medicare and Medicaid long term care facilities reported onr-star (much below average) staffing levels. More than half of the 286 were rated much below average or below average.
The staffing rating for Canterbury Rehabilitation and Health Care Center on medicare.gov below indicates that Canterbury (Lexington Court) provided to its patients only 1/3 of registered nurse minutes per resident per day required to achieve the national average of 41 RN minutes.
Plan of Correction
From that point, I change the point of reference to the Commonwealth of Virginia’s contractor, vhi.org [2] updated 3/31/2020. Note that “Information comes from data that the nursing facility reports to its state agency.”
It appears that Canterbury was required to submit a plan of correction within 10 calendar days from the date the facility received its Statement of Deficiencies, form CMS-2567 from the October 3, 2019 inspection. Federal rules require such a plan to be approved by the Virginia Department of Health. So it is reasonable to inquire if a plan of correction was submitted, whether the contents of that plan of correction were approved and whether the plan was carried out.
Conclusion
Comparing October 2019 inspection results and March 2020 self-reported staffing results, the staffing deficiencies reported by inspectors in October 2019 were either not corrected by November 1, 2019 or reappeared before the quarterly report posted on March 31, 2020.
Assessment
It cannot be acceptable that more than half of Virginia’s CMS-rated nursing homes are understaffed. We simply must require the Virginia Department of Health to do a better job.
It is even more unacceptable that the Governor, the Secretary of Health and Human Resources and the Health Commissioner do not refer to the data reflected in this essay in their thrice-weekly news conference. Their approach can be characterized as, “Who could have known?”
The answer is that they not only should have known, but should have intervened as they had the authority to do to oversee improvements in Canterbury staffing or shut it down before the COVID-19 epidemic struck that badly understaffed facility.
The data show a pattern of either disregard for the facts or incompetence. Once again, I call for the resignation or firing of Virginia’s Health Commissioner
This article has been extensively re-written since its original post in the form of an open letter. — JAB
[1] https://www.medicare.gov/nursinghomecompare/profile.html#profTab=3&ID=495272&Distn=6929.6&state=VA&name=CANTERBURY%20REHABILITATION%20%26%20HEALTH%20CARE%20CENTER&lat=0&lng=0
[2] http://www.vhi.org/Lexington%20Court%20Nursing%20and%20Rehabilitation.html?tab=&?=nh1889/