 By DJ Rippert
By DJ Rippert
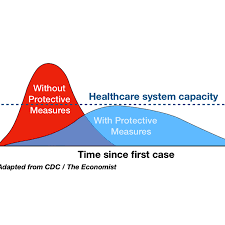
Timing. As Jim Bacon wrote, “Now comes COVID-19. Everyone is in a blind panic. The concern may be overwrought, whipped up by the media. Or maybe things could get worse than anyone could imagine. Nobody knows. Uncertainty reigns.” Jim is right. Uncertainty does reign. But what are the costs of indecision if things do get worse than anybody can imagine? The graph at the left qualitatively describes how early action can change the shape of the infection curve and avoid a peak that overwhelms our health care system. Do Virginia’s leaders understand this?
One step back, two steps forward. In 2007 the National Academy of Sciences conducted a study entitled, “Public health interventions and epidemic intensity during the 1918 influenza pandemic.” As the title implies the study compared what various governments did with the Spanish Flu pandemic against the results those governmental actions achieved. To be fair, we can look back at 1918 knowing that the influenza of that time was catastrophic. We’ll only know whether that’s true for COVID-19 at some point in the future.
Spoiler alert. The study concludes that”… cities in which multiple interventions were implemented at an early phase of the epidemic had peak death rates ≈50% lower than those that did not and had less-steep epidemic curves.” The total death rates were lower for cities that acted quickly but only by 20% not 50%.
I’ll have a cheesesteak and a Bud. Back in 1918 Philadelphia and St Louis followed very different routes regarding the speed and breadth of interventions meant to achieve “social distancing.” St. Louis got out early while Philadelphia decided to “wait and see.” From the report, “The first cases of disease among civilians in Philadelphia were reported on September 17, 1918, but authorities downplayed their significance and allowed large public gatherings, notably a city-wide parade on September 28, 1918, to continue. School closures, bans on public gatherings, and other social distancing interventions were not implemented until October 3, when disease spread had already begun to overwhelm local medical and public health resources. In contrast, the first cases of disease among civilians in St. Louis were reported on October 5, and authorities moved rapidly to introduce a broad series of measures designed to promote social distancing, implementing these on October 7.” The results?
That was then, this is now. There are countless differences between the influenza outbreak of 1918 and COVID-19 today. Perhaps the most significant is the advance of medical care. From intravenous fluids to machines which automatically oxygenate blood, today’s patient has a much better chance of survival than would have been the case in 1918. Modern healthcare does you no good if you can’t get access to it. Hence, the need to avoid overwhelming the health care system.
Paging Dr. Northam. American states are taking very different approaches to early interventions to encourage “social distancing” around COVID-9. As of now, ten states have declared states of emergency. New York has activated its national guard to isolate an outbreak cluster around New Rochelle. Virginia seems to be more in the “wait and see” camp. That could turn out to be the right decision or it could be a catastrophic error.


