In my daily update of COVID-19 statistics reported by the Virginia Department of Health (VDH) and the Virginia Hospital and Healthcare Association (VHHA), I abandoned some time ago the use of “confirmed cases” as a useful indicator of the progress of the epidemic through the general population. I turned instead to hospitalizations, which I figured was a more accurate reflection of that subset of the population displaying severe symptoms. It’s not a perfect number — it misses people who die at home or in long-term care facilities — but it’s more reliable number than confirmed tests.
Now I’m wondering about the hospital data. Either there’s something very wrong with the data, or I’ve stumbled across something very important occurring in how hospitals are responding to the virus.
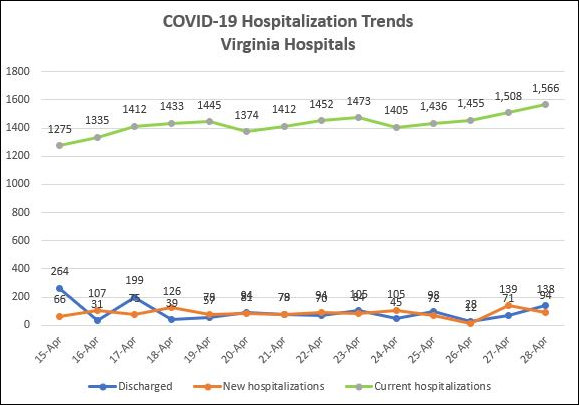
Here are the salient statistics: Over the past 13 days, the VDH has reported that 1,211 COVID-19 patients were admitted to Virginia hospitals. Over that same period, the VHHA has reported that COVID 1,318 patients were discharged. In other words, 97 more patients were discharged than were admitted. One would expect, then, that the number of patients in hospitals would have diminished by some amount.
But the reverse has happened. The total number of COVID-19 patients currently in hospitals actually increased — by 18% to 232. (See details in the graph above.)
The obvious explanation for why there are more COVID-19 patients in hospitals is that they are staying longer on average. One might conjecture that patients on average are sicker and are taking longer to recover. That would be a perfectly valid reason for an increasing hospital population.
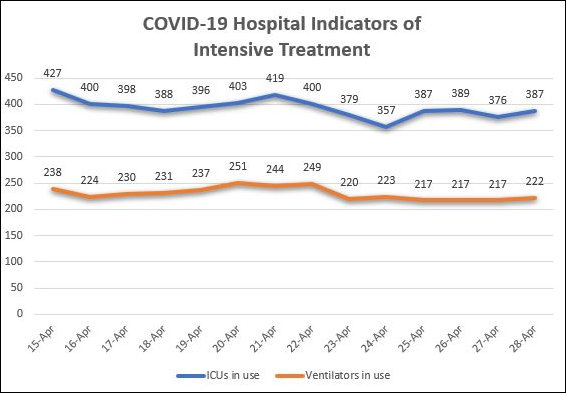
But that hypothesis flies in the face of other evidence. During the same period, according to VHHA data, the number of patients held in ICUs and using ventilators has declined slightly, as seen below.
If COVID-19 patients were sicker, we’d expect to see more of them in ICU beds and, possibly, using more ventilators. (The ventilator stats are tricky. The declining use of ventilators may reflect evolving medical opinions regarding their efficacy. The same cannot be said of ICUs, however.)
Here’s another possibility: Hospitals are are motivated for financial reasons to treat COVID-19 patients for longer periods of time because they are hemorrhaging cash like a pierced femoral artery.
In the early days of the epidemic, Virginia hospitals were concerned that the system would be swamped by a spike in the number of COVID-19 patients. The goal was to free up as much capacity as possible. Thanks to Governor Ralph Northam’s emergency shutdown measures, the patient surge never materialized. But hospitals were left stranded with loads of empty beds.
It has been widely reported that Bon Secours, Ballad Health and Carilion Clinic have instituted widespread furloughs due to declining patient counts attributable to Northam’s decree prohibiting elective surgery. Now we can add the University of Virginia Health System to the list. The hospital system, it was reported this morning, is cutting executive salaries, slashing physician compensation, reducing hours for patient-care staff, and furloughing some non-patient care staff.
Why? Because surgeries are down 70% and clinic visits are down 90%. The same scenario is playing out across much of the state.
If I were a hospital administrator distressed by empty beds, worried about literally running out of cash, and fearful that my hospital enterprise was crashing and burning, what would I do? I would urge docs to keep patients in the hospital as long as legally and ethically possible in order to generate as much revenue as possible. The increasing number of COVID-19 patients in hospitals is consistent with this theory. If I’m right, hospital stays for non-COVID patients could be lengthening as well.
I have not tested this hypothesis by checking with the hospitals themselves. Most refuse to return my phone calls during the epidemic, and those that have responded have given non-responsive, boilerplate responses. I have better things to do with the three to four hours a day I can devote to this blog than solicit no comments. But if readers can provide information that either confirms or contradicts my theory, please let me know. Either leave a comment or email me directly at jabacon@baconsrebellion.com.
(I want to credit Carol Bova for bringing issue of conflicting hospital data to my attention offline. For better or worse, the ensuing analysis is mine.)