Merriam Webster:
Pred*a*tor: (noun) one who injures or exploits others for personal gain or profit.
The most medically vulnerable of us reside in skilled nursing facilities (SNF).
Nobody plans to be there, but that is where about thirty thousand Virginians find themselves at any one time. People who are moved from hospitals to save money for the insurers but are too sick or injured to go home yet.
They are supposed to get the skilled nursing the name suggests. Many don’t.
Most are covered by Medicare. The rest by Medicaid or private insurance. It could be any one of us tomorrow.
These patients are at risk by design in some of these SNF’s. Put in danger by a perverted business model, a model that shows that returns can be juiced into double digits by stripping staff. The facilities can then be flipped in a couple of years at a profit based upon increased cash flows.
We will track their investments using government data. We will see a ritual, system-wide understaffing. We will also see that the government accumulated and publishes staffing data but there is no evidence they use it for anything.
There are nursing homes in Virginia, for example, that provide less than 30% of the registered nurse hours per patient per day that CMS assesses they require. Weekend statistics are worse. Nothing happens.
Today there are large systems not one of which is staffed to CMS norms.
There are real people who are harmed by those calculated violations. Exceptionally vulnerable people are regularly denied at least their dignity, often their health and sometimes their lives.
The owners injure and exploit patients for personal gain or profit.
They are predators.
The data. I have combined data from several different Centers for Medicare/Medicaid Services databases to examine the issues and identify the worst actors, both investors and managers.
Those databases were downloaded within the past week.
We will focus on staffing because it is a leading indicator of future performance.
It is also where profits can be made by the unscrupulous by cutting staff, their biggest expense.
Federal law requires all nursing homes to provide enough staff to safely care for residents. However, there is no current federal standard for the best nursing home staffing levels.
The CMS staffing rating takes into account differences in the levels of residents’ care needs in each nursing home.
For example, a nursing home with residents that have more health problems would be expected to have more nursing staff than a nursing home where the residents need less health care.
Each nursing home reports daily staffing hours to Medicare. Medicare calculates a ratio of staffing hours per resident day, the percent of nurse staff that stop working at the facility (turnover), and the number of administrators who have left the facility within a given year. These types of staff are included in the nursing home staffing information:
- Registered Nurse (RN)
- Licensed Practical Nurse (LPN) and Licensed Vocational Nurse (LVN)
- Certified Nurse Aides (CNAs)
- Physical therapist (PT)
- Administrator
All of those personnel are licensed by the Commonwealth.
There is considerable evidence of a relationship between nursing home staffing levels and resident outcomes.
The CMS Staffing Study, among other research, found a clear association between nurse staffing ratios and nursing home quality of care. There is also a growing body of evidence on the relationship between staff turnover and resident outcomes, with higher turnover associated with poorer quality of care. [Emphasis added.]
The staffing rating is based on six measures and are as follows:
• Case-mix adjusted total nurse (RN, LPN/LVN, aide) staffing levels (hours per resident per day);
• Case-mix adjusted RN staffing levels (hours per resident per day);
• Case-mix adjusted total nurse (RN, LPN/LVN, aide) staffing levels (hours per resident per day)
on the weekend;
• Total nurse turnover, defined as the percentage of nursing staff that left the nursing home over a
twelve-month period;
• Registered Nurse (RN) turnover, defined as the percentage of RN staff that left the nursing home
over a twelve-month period;
• Administrator turnover, defined as the number of administrators who left the nursing home over a
twelve-month period.Staffing data are adjusted for the needs of the nursing home residents.
CMS calculates case-mix adjusted hours per resident day for each facility for each staff type using this formula:
Hours Adjusted = (Hours Reported/Hours Case-Mix) * Hours National AverageThe source for reported staffing hours is the Payroll-Based Journal (PBJ) system. These data are submitted quarterly and are due 45 days after the end of each reporting period. Only data submitted and accepted by the deadline are used by CMS for staffing calculations and in the Five-Star Rating System. The resident census is based on a daily resident census measure that is calculated by CMS using MDS assessments.
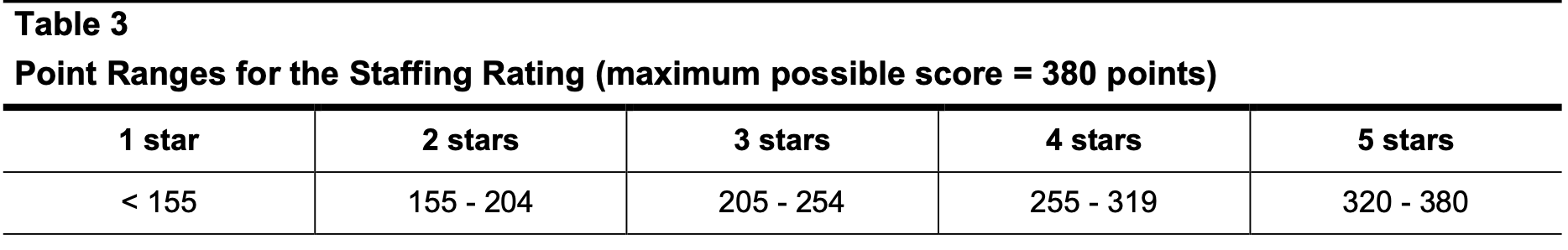
A nursing home receives points based on how they perform on each staffing measure (some measures are weighted more than others). The points for each measure are totaled, and the nursing home is assigned ratings based on thresholds for each rating category. Nursing homes may be assigned a 1 star rating if they don’t have an RN onsite every day, don’t submit staffing data, or if their data can’t be verified [author note: verified with payroll data].
The understaffing business models raise a lot questions.
- About ethics;
- About the actions or inactions of state regulators and licensors of nursing homes;
- About the actions or inactions of state licensors of nursing home administrators;
- About insurance reimbursements with federal funds for services not properly rendered and documented with detailed evidence of regulation violations;
- About potential legal action by state and federal prosecutors for patterns of such violations including a clear conspiracy evident in the ownership records; and
- About why the tort bar has not yet been able to sue these groups out of the nursing home business.
They constitute scandals at least.
Whether they also constitute criminal conspiracies is for law enforcement to decide.


Leave a Reply
You must be logged in to post a comment.