In the sometimes murky world of diagnosis and treatment of gender dysphoria in children and adolescents, the following steps generally but not always occur in order, with each potentially serving as an off-ramp:
- Diagnosis;
- Mental heath support;
- Social transition;
- Puberty blockers;
- Cross-gender hormones; and,
- Surgery; often but not always waiting for surgery until a child reaches the age of majority.
That list gets dangerous when it gets to step 4.
What UVa Children’s Hospital requires is the diagnosis before it can proceed. It cites a list of “gender affirming” medical professionals to whom it will refer patients for that diagnosis. Many of them are on staff I hope they are not as forward-leaning on this diagnosis as their advertising suggests.
The home page of the clinic lists the following services in order:
- Puberty blockers that delay sex-related physical changes;
- Cross-sex hormones, like testosterone and estrogen;
- Referrals for gender-affirming surgeries and voice therapy;
- Education about sex and contraception;
- Referrals for therapy to help manage anxiety, depression, and ongoing emotional issues;
- Help finding resources in the community.
I think those are presented in the wrong order. Therapy should be first. More on that later. Yesterday we discussed puberty blockers.
Today we will focus on cross-gender hormones.
Diagnosis, mental health support and social transition. Cleveland Clinic has a web page titled: “Transgender: Ensuring Mental Health.”
(Gender dysphoria) describes a sense of unease regarding the mismatch between assigned sex and gender identity — and it can occur at any point during life, from childhood to adulthood. Left untreated, gender dysphoria can lead to severe emotional and psychological distress.
Gender dysphoria can lead to other mental health challenges, including:
- Anxiety;
- Depression, sadness or a sense of loss;
- Negative self-image or poor self-esteem;
- Post-traumatic stress disorder (PTSD);
- Shame;
- Social isolation.
Read Cleveland Clinic’s: “How can a mental healthcare provider help me or my transgender child? and “How can I help support my transgender child’s mental health?”
Good advice there.
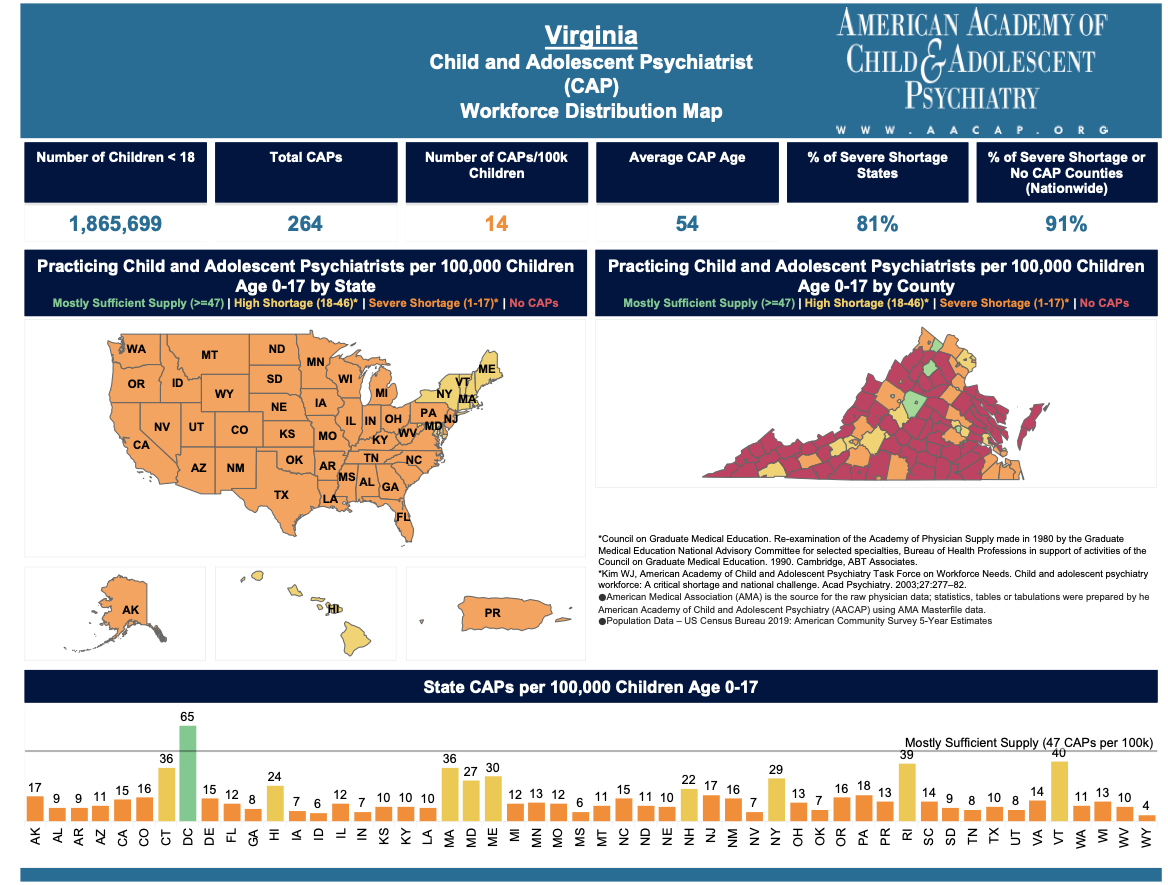
UVa Children’s offers therapy with staff psychiatrists. There are enough child and adolescent psychiatrists (CAP) in that area precisely because of the hospital. It would smooth some of the sharp edges of their teen and adolescent transgender clinic pages if they emphasized those services up front.
Other localities in Virginia are severely short of CAPs.
Puberty blockers.
The use of puberty blockers — a family of medications known as gonadotropin-releasing hormone (GnRH) analogs — in gender dysphoria treatment represents an off-label use of these powerful hormones.
There are significant FDA warnings for their on-label use. I reviewed them yesterday.
But there is no scientific data that meets FDA requirements to understand the long-term effects of those hormones when used for gender dysphoria.
Cross-gender hormones. Used in an adolescent, hormone therapy typically begins at age 16, before the development of secondary sex characteristics that have been suppressed by puberty blockers.
There are four areas where changes occur as cross gender hormone therapy progresses. Physical, emotional, sexual, and reproductive. They vary between masculinization and feminization therapies.
Estrogen is associated with thromboembolic disease, macroprolactinoma, breast cancer, coronary artery disease, cerebrovascular disease, severe migraine headaches, and potentially, irreversible infertility.
Testosterone use in female-to-male therapy carries the risk of breast or uterine cancer, erythrocytosis, and severe liver dysfunction.
Surgical sterilization of minors requires a court order in Virginia. Medical sterilization in this procedure does not.
Off label. Like puberty blockers, transgender hormone therapy for adolescents is an off-label use of the hormones.
Off-label means that the FDA has not approved the hormones for the uses to which the physicians are putting them. Not approved does not mean illegal, but by definition means that they are experimental in our system of medicine.
Guidelines. The medical guidelines for endocrinologists are found in Endocrine Treatment of Gender Incongruent/Gender Dysphoric Persons: An Endocrine Society Clinical Practice Guideline Summary of Recommendations recommends against puberty blocking and gender-affirming hormone treatment in prepubertal children with GD/gender incongruence.
For treatment of adolescents those same guidelines recommend:
2.1. We suggest that adolescents who meet diagnostic criteria for GD/gender incongruence, fulfill criteria for treatment, and are requesting treatment should initially undergo treatment to suppress pubertal development.
2.2. We suggest that clinicians begin pubertal hormone suppression after girls and boys first exhibit physical changes of puberty.
2.3. We recommend that, where indicated, GnRH analogues are used to suppress pubertal hormones.
2.4. In adolescents who request sex hormone treatment (given this is a partly irreversible treatment), we recommend initiating treatment using a gradually increasing dose schedule after a multidisciplinary team of medical and MHPs has confirmed the persistence of GD/gender incongruence and sufficient mental capacity to give informed consent, which most adolescents have by age 16 years. [Editor’s note: this is a disconnect with the age of majority in Virginia which is 18.]
2.5. We recognize that there may be compelling reasons to initiate sex hormone treatment prior to the age of 16 years in some adolescents with GD/gender incongruence, even though there are minimal published studies of gender-affirming hormone treatments administered before age 13.5 to 14 years. As with the care of adolescents ≥16 years of age, we recommend that an expert multidisciplinary team of medical and MHPs manage this treatment.
2.6. We suggest monitoring clinical pubertal development every 3 to 6 months and laboratory parameters every 6 to 12 months during sex hormone treatment.” [Emphasis added.]
As far as I know, those guidelines have no legal status in Virginia, but it is useful to understand what UVa Children’s endocrinologists have as reference.
Objections. There are Virginians who support wholeheartedly what UVa Hospital is doing in these cases. They most commonly cite the threat of suicide if such measures are not taken.
On that specific point, there are others who worry that, given the severe shortage (14 actual vs. 47 required per 100,000 children) of pediatric psychiatrists in Virginia, the appropriate mental health measures may not be taken or available in some cases.
In the face of that shortage, we have no public data on the degree to which mental health support measures are accessed in minor patients treated with hormones for gender transition in Virginia.
I suspect it would take a state inspection to determine that.
There is also a litany of medical, ethical and moral objections to the use of powerful hormones for gender changes in minors.
- Lots of people have a problem with the experimental status of the use of hormones in these applications.
- Many pediatricians and pediatric endocrinologists offer medical ethics objections. First do no harm. They object to the acceptance by their national associations of practices unsupported by scientific evidence of long-term effects.
- Some medical and legal objections also center on the inability of children to possess sufficient brain development and experience to make risk-reward decisions of this magnitude and consequence. While proponents cite the “desires” and “needs” and “agreement” of some minors for these medical transitions, Virginia’s law defines the age of majority as 18. They are legally incapable of making such decisions.
- Then there are the moral objections of many about doing this to children.
So parents are required to decide.
They must be given all of the information necessary to make an informed decision, especially including the dangers, including risks of irreversibility of some of these treatments.
It is up to the Virginia Department of Health, which has oversight over the University of Virginia Hospital, a state institution, to determine whether that hospital is practicing medicine within the boundaries of state standards in gender transition of minors. I suspect it is. I also suspect there may be gaps in those standards.
The mission of the Department of Health Professions is:
to ensure safe and competent patient care by licensing health professionals, enforcing standards of practice, and providing information to health care practitioners and the public.
It is up to that department to provide that information and assure the public in this case.
Assuming that is done, the question then is whether the medical, ethical, and moral objections rise to the level that these experimental treatments should be regulated or stopped by law in Virginia
Once oversight is complete, the Governor and General Assembly can determine whether new laws are needed.