The The Virginia Mercury has published a well-reported article today about the challenges of addressing the spread of COVID-19 in Virginia nursing homes, which account for 57% of all COVID deaths in the state.
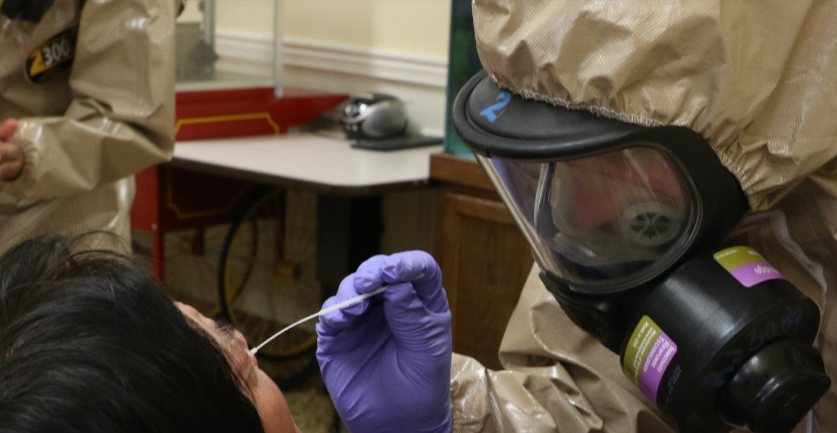
The Virginia Department of Health is gearing up for a massive expansion of testing at the nursing homes. Drawing upon funding through the Virginia National Guard, VDH has already begun performing broad baseline testing, which it refers to a “point prevalence” surveys.” Of the state’s 287 nursing facilities, only 42 have been tested. Some facilities have been conducting their own testing at their own expense. However, some facilities have resisted baseline testing, presumably on the grounds that tests would reveal the presence of asymptomatic employees, thus exacerbating staffing problems.
Now, following the issuance of federal Centers for Medicare & Medicaid Services (CMS) guidelines, VDH expects to begin implementing recommendations as soon as it can “work through the guidance an turn it into something more useable,” in the words of Sarah Lineberger, director of the agency’s health care-associated infections program.
VDH likely will ask every facility to conduct a baseline test of all residents and staff members, then test staff on a weekly basis thereafter. It is widely assumed that asymptomatic staff are primarily responsible for bringing the virus into nursing homes. The big question, as always, is who pays?
At $100 to 175 per test, The cost of tests for 30,000 nursing home residents and 30,000 employees would run between $6 million and $10.5 million. And that doesn’t include the significant cost in staff time and personal protective equipment (PPE) to administer the tests. It is not known how long the funding will last for the National Guard to continue testing. Medicare reimburses up to $100 per test for patients, but nothing for staff.
Numerous nursing homes have reported difficulty in acquiring PPE for staff, although the number reported on the Virginia Hospital and Healthcare website has declined in recent days. Only seven facilities reported difficult obtaining N95 masks and nine acquiring isolation gowns.
Secretary of Finance Aubrey Layne says that the price tag attached to expanded testing has become the main sticking point for VDH. The Virginia Department of Medical Assistance Services, which administers the Medicaid program, upped its reimbursements by $20 per patient per day in April. The money was freed up by the ban on elective procedures. That savings will continue to go to nursing homes through June, but he’s not sure if the state can maintain the funding after that.
Another challenge is that nursing homes haven’t been able to get money from federal or state assistance. Virginia’s hospitals have received $170 million in federal helicopter dollars, but the nursing homes nothing. States are forbidden from directing coronavirus relief dollars to replace lost revenues. Also, Layne says, some people have expressed concerns with sending more money to facilities owned by for-profit companies with poor records of care.