A challenge to Virginia’s largest not-for-profit health systems: just do it.
Take the lead.
Note the medically underserved areas (MUAs) next to your headquarters and flagship hospitals and provide primary care in those locations.
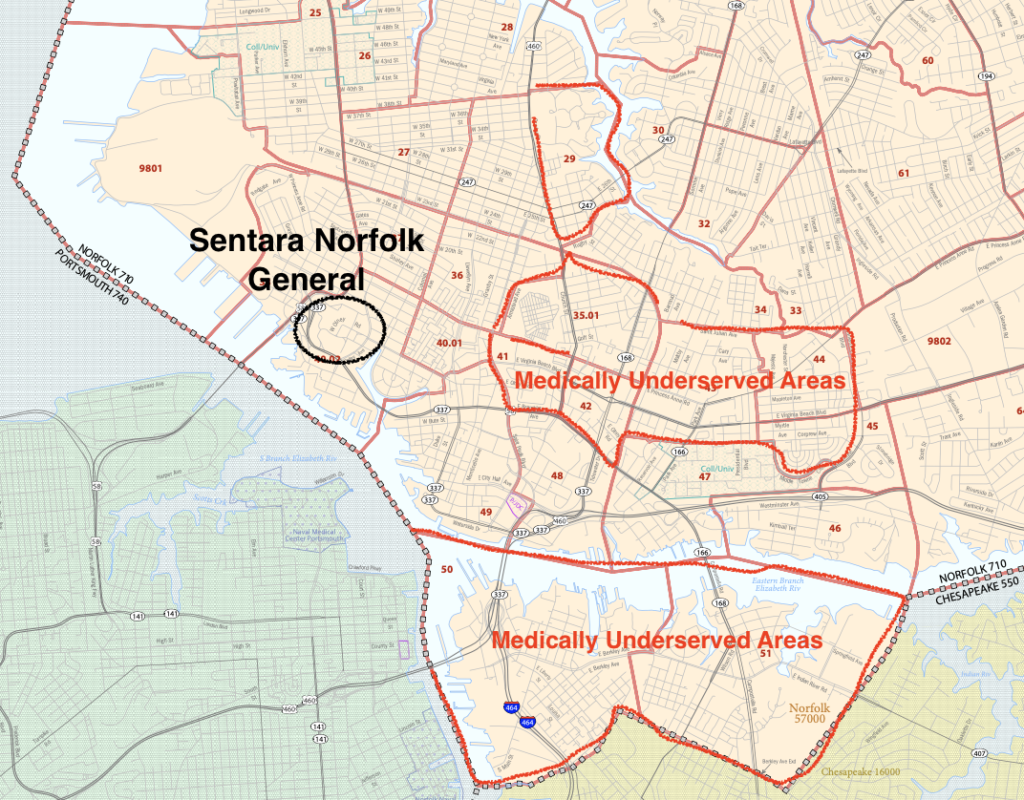
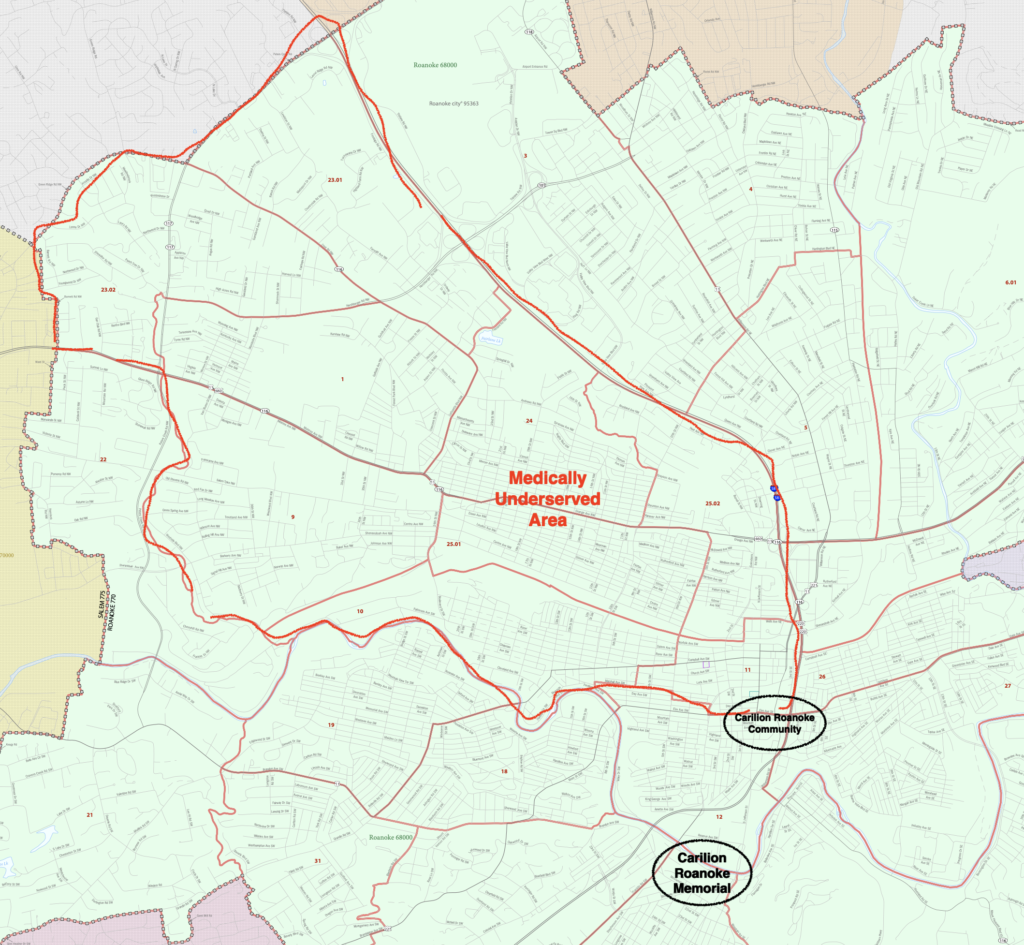
Virginia has federally-designated MUAs in Arlandria (INOVA), Norfolk (Sentara), Roanoke (Carilion) and Lynchburg (Centra). Those health systems are each headquartered in those cities.
- Arlandria is four miles from INOVA Alexandria Hospital. It was just designated in 2022.
- The medically underserved census tracts in Norfolk (pictured above) are closer than that to Sentara’s flagship Norfolk General Hospital. Those are just the worst of them. Eight more Norfolk census tracts made the list. Pretty much every poor area of the city. I got tired of outlining them. But you get the idea. Originally designated in 1994. Updated in 2009.
- Carilion Roanoke Community Hospital is right at the edge of that city’s underserved tracts. Originally designated in 1998. Updated in 2012.
- Underserved areas in east Lynchburg are in the service area of Centra’s flagship Lynchburg General Hospital. Designated in 1994. Updated in 2011.
The leadership of those health systems drive through those areas on the way to work.
Not-for-profit health systems conduct community health needs assessments (CHNA) once every three years to meet federal and state requirements. The CHNAs of those four health systems have recognized that those areas are underserved in primary care for a very long time.
Time for them to take the lead to provide primary care in communities a bicycle ride from their headquarters and major hospital facilities.
Then as a state we can move forward into more challenging areas.
Note Roanoke’s medically underserved areas.
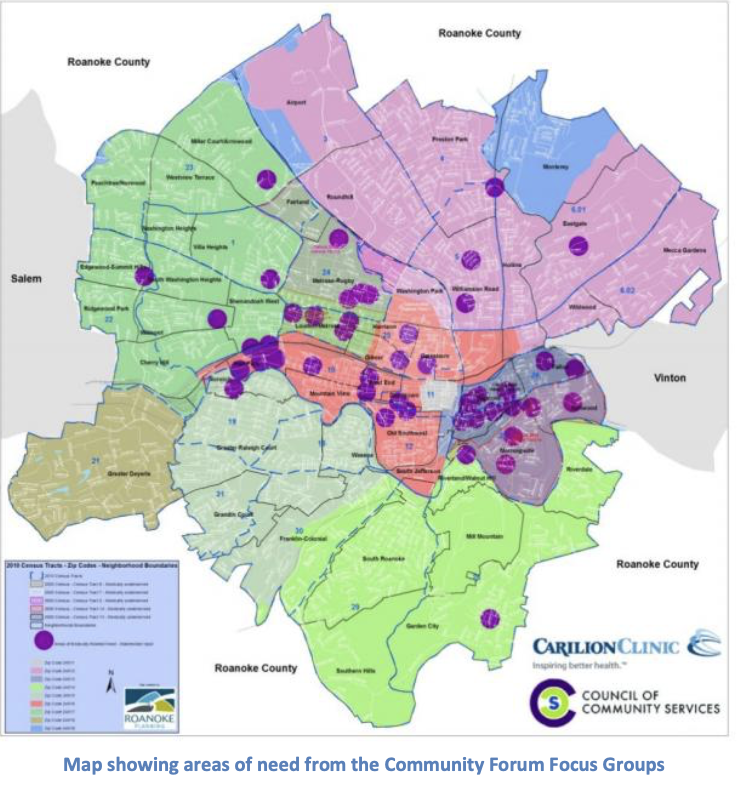
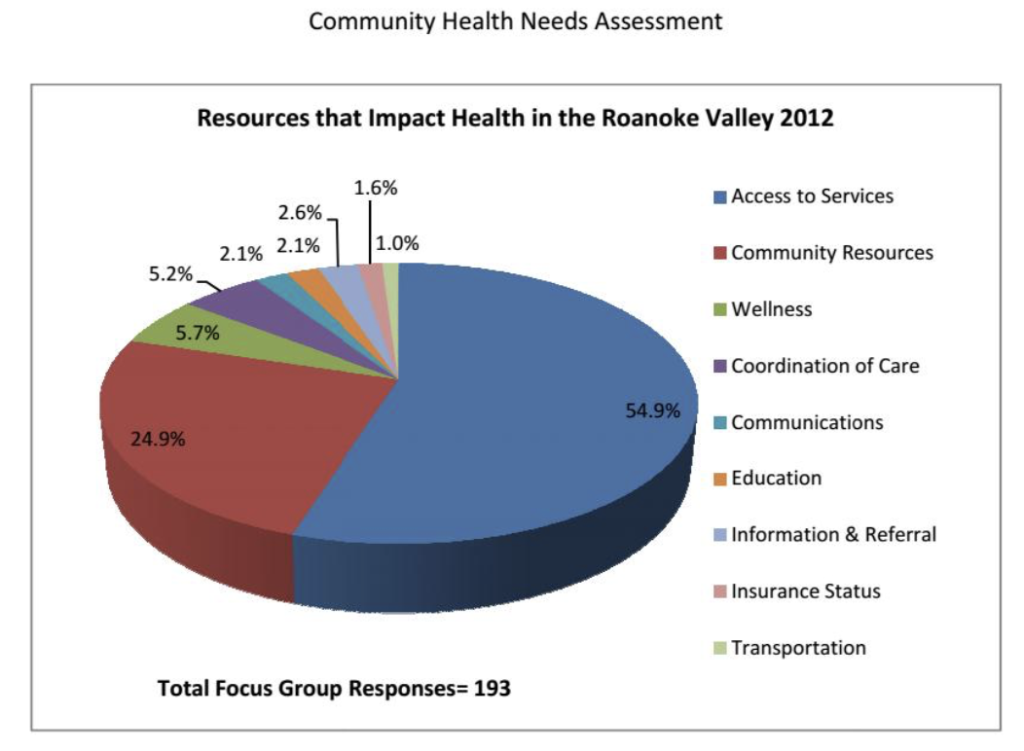
Carilion’s Roanoke CHNA in 2012 illustrated the need (below).
It also illustrated what was needed – access to services
So, we have to ask why, more than a decade on, those same areas are still designated as medically underserved in primary care.
Let’s say for illustration that a few of the answers include:
- the area is dangerous;
- it’s tough to find suitable medical office locations;
- reimbursements from Medicaid and Medicare are paltry;
- patients cannot be depended upon to show up to appointments;
- language barriers.
I don’t know if these challenges apply to those census tracts in Roanoke specifically, or in the other three cities, but we’ll use them for illustration.
- The area is dangerous. Get the Mayor, the city manager and police to commit to protect medical office locations. Think outside the box. Start primary care – medical and dental – with pediatrics. Get the word out that the office initially is just for kids. Then, when that gets established, add geriatrics. That sort of thing.
- Suitable office locations. At least two options to keep costs down and add security at no cost to the healthcare providers:
- Build a purpose-built facility on school grounds. That is a “thing” now called community schools. Use steel buildings to keep the costs down.
- Have the city donate a couple of the many properties in the tracts that it has seized for various reasons and convert them to medical offices.
- In both cases use metal detectors at entrances manned during working hours by police.
- Medicaid and Medicare reimbursements and healthcare workers pay. Work with DMAS to see what special payment and educational debt reimbursement programs can be leveraged. Pay healthcare workers what it costs. The travel nurse program worked, and these four areas don’t require overnight travel.
- Patients cannot be depended upon to show up. Ask DMAS to get the Medicaid Managed Care contractors they pay to address that to, well, address it. Get social services involved as necessary.
- Language barriers. Work with social services and the school nurses to help address that. Employ bi-lingual physicians and nurses. If necessary, bring in native speakers of the requisite languages that are graduates of foreign medical schools licensed by the Accreditation Council for Graduate Medical Education (ACGME).
Partners for the health systems:
- Virginia Secretary of Health and Human Resources. He controls all of the state health care, health professions and social services agencies. His agencies are already helping Petersburg.
- City officials. Mayor, City Manager, School Board Chair, Police Chief.
- Community organizations including neighborhood groups and churches.
What I have just described is substantially how Health Enterprise Zones work. No need to call them that in this case.
Make it an initiative led by the health systems and supported by government.
Given the resources, political power, financial strength and management expertise of those four large health system monopolies, such programs will work if they get behind them.
These four cities are where Inova, Sentara, Centra and Carilion are headquartered.
There are large swaths of other urban areas that are similarly underserved. Hampton and Newport News, for example, are adjacent and share 23 census tracts that are underserved.
Speaking of Sentara, which I occasionally do, there are census tracts in Virginia Beach, tracts in Chesapeake adjoining Norfolk, and the entire city of Suffolk on the list.
Getting healthcare workers to live in other areas of the state that are rural presents a different set of challenges, mostly focused on smaller populations to be served and whether healthcare workers wish to live there, but those also must and can be addressed.
The program in four cities recommended here should be the easy part.