by James A. Bacon
In Fairfax County, Latinos comprise about 16% of the population yet 60% of the county’s COVID-19 cases. A recent health study described the neighborhood of a Hispanic woman profiled by WAMU, Ana Mejia, as an “island of disadvantage.” A third of the neighborhood’s children live in poverty, and more than half the residents are uninsured. Workers are more likely to be exposed to infection at work and then bring it home to their cramped apartments.
You know the routine. The wind-up: WAMU quotes Luis Aguilar, head of immigrant advocacy group CASA Virginia, as saying that Latinos are disadvantaged because many undocumented immigrants do not qualify for Medicaid, unemployment benefits or stimulus checks from the federal government. And the pitch: “The approach of relying on non-profits to step in during a pandemic … there needs to be a lot more from the local government,” he says.
In other words, there needs to be more money from taxpayers. “Fairfax County is one of the top five wealthiest counties in the United States of America, and if Fairfax can’t afford testing for its low-income residents, that would really surprise me,” the article quotes state Sen. Scott Surovell, D-Mount Vernon, as saying.
You have to read deep into the article before you run across this tidbit: County epidemiologist Rene Najera said he noticed one encouraging sign. Spanish-speaking patients seem to be surviving the disease. “We’re talking about a generally younger population, maybe a little bit more resilient. It might be getting them to the hospital but it might not be killing them at a higher rate.”
Indeed, the statistics are startling. While Hispanics are significantly more likely than the general population to have confirmed cases of COVID-19, they are less likely to be hospitalized, and far less likely to die. Talk about disparities!
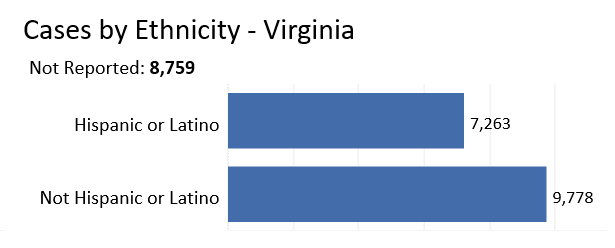
Here’s how the Virginia Department of Health dashboard breaks down confirmed COVID-19 cases by Hispanic vs. non-Hispanic ethnicity:
Hispanics account for about 15% of Virginia’s population but nearly 43% of all COVID-19 cases. The disparity in infection rates is roughly comparable statewide to what it is in Fairfax County. But a funny thing happens when you look at hospitalization rates.
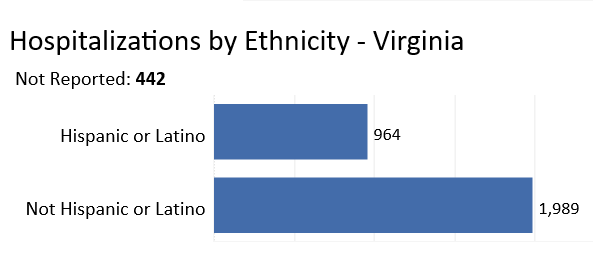
While 43% of COVID-19 cases are Hispanic, only 32% of hospital admissions for the disease are Hispanic. And even more remarkably….
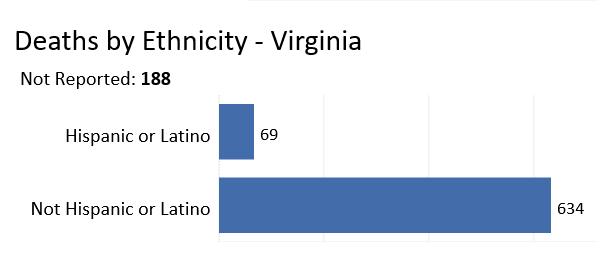 … Only 11% of those who die from COVID-19 are Hispanic! As a percentage of the population, fewer Hispanics have died from the virus than non-Hispanics.
… Only 11% of those who die from COVID-19 are Hispanic! As a percentage of the population, fewer Hispanics have died from the virus than non-Hispanics.
How do those numbers comport with the dominant media/ruling class narrative that view every issue through the lens of racial/ethnic disparity, attributes disparities between groups to differential access to public resources, and calls in every case for more spending by one level of government or another?
Here’s my first question: If Latinos are so dramatically under-served that Fairfax County needs to step in and spend more money on testing in their neighborhoods, how do we know that so many Hispanics have contracted COVID-19? Those people had to be tested, right? So, clearly a lot of testing has occurred. If you want to make the case that there is a disparity in access to testing, show me the data that shows Hispanics are being tested less frequently. The WAMU story presents none whatsoever. It’s possible that Hispanics are, in fact, less likely to be tested, but no one has presented any evidence to prove that it is. I do not accept such sweeping assertions as an article of faith that needs no proof.
Here’s my second observation: If Hispanics suffer from such a differential access to Virginia’s health care system, how come so many manage to get into hospitals? Is the fact that they are being hospitalized at higher rates than the rest of the population a sign of unequal access to healthcare? (The question of who pays for that access is a different question for a different discussion.)
And a third observation: How come so few Hispanics, relatively speaking, are dying from the disease? Clearly, age is a factor. Hispanics in Virginia are significantly younger than other Virginians — a median age of 27 compared to 38. Deaths from the virus are highly correlated with age, and the population of over-80 Hispanics in Virginia is very small. On the other hand, does age account for the full difference? Do Hispanics have other characteristics — for example, fewer co-existing conditions that also affect mortality rates? Do Hispanics do something — do they have more nutritious diets, do they work more outdoors — that might make them more resistant?
There are many potentially useful questions we could be asking but aren’t because the media and public health authorities are locked into a particular paradigm for viewing the world. The priority in fighting the COVID-19 pandemic should be halting the spread and saving lives, not re-affirming the Oppression Narrative.