by James C. Sherlock
by James C. Sherlock
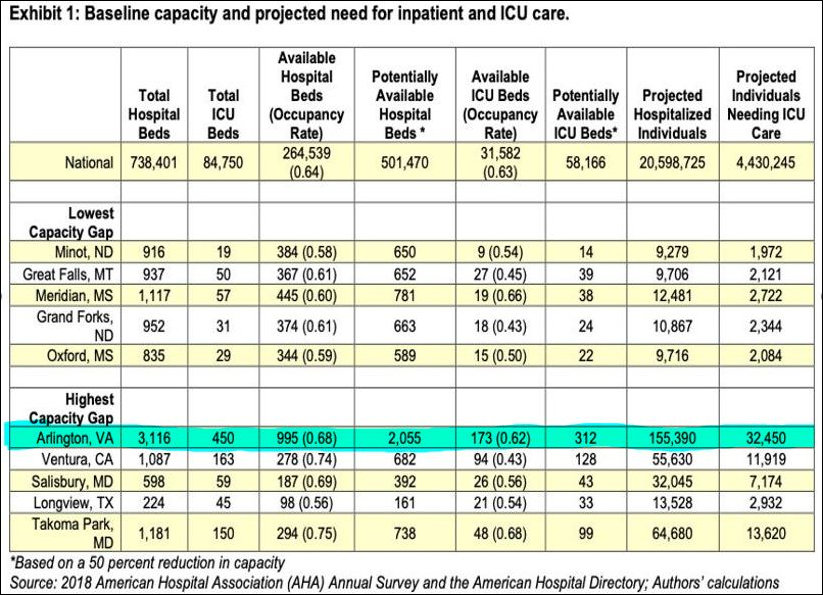
Every time the discussion in this space turns to COPN and its relationship to lack of capacity to deal with COVID-19, some commenters accuse the authors of these columns of favoring nonsensical solutions such as forcing hospitals to build excess capacity. Those same commenters then reject those concepts as unworkable. That is the very definition of a straw man. Unfortunately it mirrors what will be a all-hands-on-deck attempt by Virginia’s hospitals and their lobbyists to sweep the damning history of COPN under the rug in the 2021 General Assembly.
No author has suggested building excess capacity to “sit idle”; what we each have suggested is to let commercial businesses, both for-profit and not-for-profit, build what they think is necessary where the think it is necessary without state interference other than enforcement of antitrust and licensing laws. Every one has carefully wrought business plans. If some misjudge demand, then either they will fail or their competitors will. If it existing provider facilities fail, that means that the new entrant offered better care or a better price or both. Any restrictions on such creative destruction must be swept away for the good of all of us.
What about day-to-day non-crisis access for the poor?
“Recent research by Thomas Stratmann and Jacob Russ demonstrates that there is no relationship between CON programs and increased access to health care for the poor. There are, however, serious consequences for continuing to enforce (COPN) regulations. In particular, for Virginia (COPN restrictions) could mean approximately 10,800 fewer hospital beds, 41 fewer hospitals offering magnetic resonance imaging (MRI) services, and 58 fewer hospitals offering computed tomography (CT) scans. For those seeking quality health care throughout Virginia, this means less competition and fewer choices, without increased access to care for the poor.”[1] Continue reading →