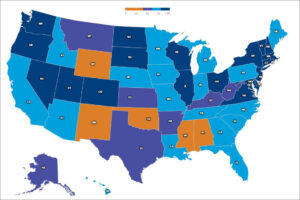
Palliative care grades by state. Source: released 2019 “State-by-State Report Card on Access to Palliative Care in our Nation’s Hospitals”
by James A. Bacon
There are many ways to gauge the quality and cost-effectiveness of Virginia’s hospitals. One is to measure cost and efficiency. Another is to track mortality rates and re-admissions. Yet another is to rate patient satisfaction. You can find these metrics on the Virginia Health Information website.
But health care is a phenomenally complex business, and many other aspects of hospital care are measurable. In a recent press release, the Virginia Hospital & Healthcare Association (VHHA) pointed out, for instance, that Virginia is one of 20 states (and Washington, D.C.) to earn an “A” for palliative care, based on a study by the Center to Advance Palliative Care and the National Palliative Care Research Center.
What is palliative care? It is, according to the report, “specialized medical care for people living with a serious illness. It is focused on providing relief from the symptoms and stress of the illness. The goal is to improve quality of life for both the patient and the family. Palliative care is based on the needs of the patient, not on the patient’s prognosis. It is appropriate at any age and at any stage in a serious illness.”
Having witnessed the lingering deaths of a step mother and father-in-law in recent years, I get it. The goal should not be to prolong life at any cost but to improve the quality of life that remains.
The VHHA also points to a study, the 2019 Leapfrog hospital safety grades to show that Virginia ranks second in the nation for “patient safety.” By safety, Leapfrog means protecting patients from errors, injuries, accidents, and infections in the hospital. I have to say, if I go into a hospital for treatment of an illness, I don’t want to acquire additional maladies while I’m there. As the Hippocratic oath says, “First, do no harm.” Pretty basic, but keeping hospitals safe is easier said than done. (See Virginia hospital scores here.)
Obviously, the VHHA brought these reports to the public’s attention because they make Virginia hospitals look good. Fair enough. They deserve credit where credit is due.
Hospitals are the core institutions of Virginia’s health care system around which all other components revolve. They deserve a lot more attention and analysis — the good along with the bad — than Virginia’s shriveled newsrooms can give them. The problem isn’t just the declining number of journalists, however. Newsrooms still cover health care. They just treat health care mainly as an issue of access and victimhood, so Virginians get mostly articles about Medicaid expansion, hospital closures, hospital lawsuits against patients who can’t pay, and the like.
But healthcare affects everyone, not just the poor and dispossessed. The average employer-provided health care policy now costs a typical American family $20,000 a year — not counting deductibles and co-pays. The cost of healthcare is a huge burden to middle-class families. Why? What is driving costs so high? What is being done in the realm of public policy to boost productivity and improve outcomes to the benefit of all? Is anyone even asking those questions?
Virginians celebrate the successes of the big health care systems — VCU, UVa, Inova, Sentara, Carilion — in increasing the volume of R&D grants as a sign of economic vitality, which, from one perspective, it is. But no one is asking where the money that funds those successes come from. How much (if any) comes from over-charging students enrolled in schools teaching the medical professions? How much comes from over-charging patients? How much of the cost of private health policies represents hidden transfer payments to Medicare and Medicaid patients?
Finally, there is the political economy angle. How powerful and influential is the hospital industry in Virginia? Health care entities have given $9.5 million in campaign contributions so far this electoral cycle, according to the Virginia Public Access Project, ranking it behind only the real estate/construction and retail industries. What legislation do health care entities want, and who benefits? Are they advancing socially beneficial reform or obstructing it?
There is so much that we, as members of the public, do not know. A wealth of data is available to anyone who wants to look at it, but few have the inclination or time to do it. The blind are leading the blind.


