by Carol J. Bova
After a review of over 15,000 nursing home reports submitted to the Centers for Medicare and Medicaid (CMS), Brian E. McGarry, David C. Grabowski, and Michael L. Barnett published a paper in Health Affairs on August 20th. In “Severe Staffing and Personal Protective Equipment Shortages Faced by Nursing Homes During the COVID-19 Pandemic,” they concluded, “Despite intense policy attention and mounting mortality, the shortages have not meaningfully improved from May to July of 2020.”
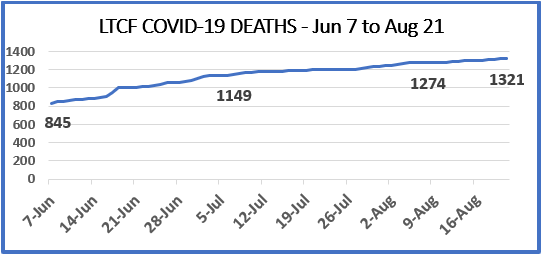
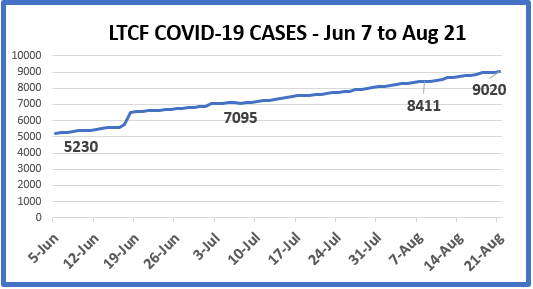
While six fewer Virginia nursing homes reported nursing staff shortages as of August 9, there were more reports of all other staff shortages and supplies of Personal Protective Equipment (PPE) between the weeks ending June 7 and August 9 according to the CMS COVID-19 Nursing Home Dataset. Meanwhile, COVID-19 cases and deaths continue to rise.
On June 8th, I wrote to COVID19JIC@vdem.virginia.gov, healthandhumanresources@governor.virginia.gov, and Tammie Smith at the Virginia Department of Health. She replied to my question of whether the Virginia Department of Health reviewed the dataset and what action they took, if any, in regard to the PPE shortages reported May 31. Her response was:
Long term care facilities are encouraged to practice PPE conservation per CDC guidance and to reestablish their PPE supply chains; access has improved recently. Those unable to source PPE through their regular supply chains routinely contact the State Unified Command for assistance.
Publicly provided PPE is distributed regularly to these facilities to ensure optimum safety in response to the COVID-19 pandemic. PPE requests are coordinated and sent to the Virginia Emergency Support Team (VEST) through their Regional Healthcare Coalitions.
Guidance information for nursing homes is here https://www.vdh.virginia.gov/content/uploads/sites/182/2020/05/VirginiaLongTermCareFacilityTaskForceCOVIDPlaybook.pdf
Two months later, there are still 57 Virginia nursing homes reporting PPE shortages, 20 without a current supply of N95 masks and 13 of those with no surgical masks either, and one without any hand sanitizer.
The system isn’t working. Whether there are additional failures in infection control procedures is to be seen as normal nursing home inspections resume. But there is no excuse for the Commonwealth’s failure to ensure adequate supplies of PPE. If owners are at fault, fine them or take other actions. The Commonwealth needs to act now.
As McGarry et al said, “Unless these shortages are prioritized by policymakers, long-term care residents will continue to be at a great disadvantage in the pandemic.”
As of August 21, 14.6% of all LTCF (long-term care facility) cases (1,321 of 9,020) have ended in death, and represent 54.1% of all COVID-19 deaths in Virginia. By comparison, correctional facilities have seen a total of 16 deaths. Our nursing home residents do not deserve a death penalty for being in a nursing home without adequate supplies or staff.