by James A. Bacon
The United States spends more money per capita on health care than any other nation yet Americans have a shorter life expectancy than citizens in 16 countries with advanced economies. The conventional wisdom blames the fragmented and dysfunctional American health care system. A new National Research Council and Institute of Medicine report, “Shorter Lives, Poorer Health,” doesn’t let the health care system off the hook. But it does point out that the behavior of Americans explains much of the difference .
“The problem is not simply a matter of a larger uninsured population or even of social and economic disadvantage,” states the report foreword . “It cannot be explained away by the racial and ethnic diversity of the U.S. population. … The U.S. disadvantage is expressed in higher rates of chronic disease and mortality among adults and in higher rates of untimely death and injuries among adolescents and small children.”
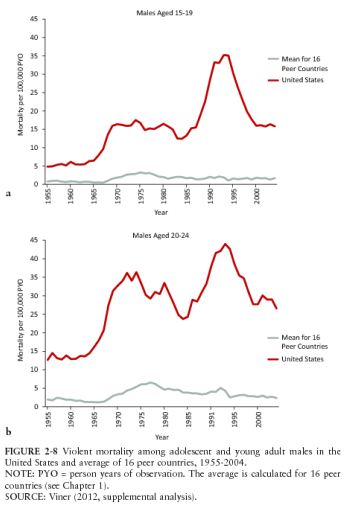
American rate of young male mortality from violence shown in red. Rate for 16 peer nations shown in gray.
In other words, Americans are far more likely to kill each other with guns and die in automobile accidents. Americans also experience a higher infant mortality rate, higher mortality rates from alcohol and drugs, a higher rate of HIV infection and a higher rate of sexually transmitted diseases. The U.S. blows out other nations in the number of “years of life lost” by males before age 50.
“Concerted action is required on many levels of society if the nation is to change the conditions described here and to give the people of the United States — particularly the nation’s children — the superior health and life expectancy that exist elsewhere in the world,” writes Steven H. Woolf, chairman of the panel of authors and a professor of family medicine at Virginia Commonwealth University.
Lifestyle and environmental factors play a significant role. Just four health behaviors — tobacco use, unhealthy diet, physical inactivity and problem drinking — are associated with 40% of all deaths in the U.S. While Americans actually smoke and drink less than citizens of peer countries, the U.S. has the highest obesity rate, which is strongly associated with diabetes, heart disease and disability. Although these problems are most pronounced among “socioeconomically disadvantaged” groups, even “advantaged” Americans fare worse.
If Americans make it to age 75, they actually have a higher survival rate than other countries. The U.S., says the report, “has higher rates of cancer screening and survival, better control of blood pressure and cholesterol levels [and] lower stroke mortality.” These indicators suggest that the U.S. health care system out-performs those of other countries in important ways.
While the U.S. health care system also has shortcomings, most notably the fragmentation of delivery and barriers to access for lower-income Americans, the authors are cautious about blaming health disparities on those flaws. “One difficulty in attributing the U.S. health disadvantage to deficiencies in public health or medical care system is that countries with better health outcomes lack consistent evidence that their system systems perform better,” states the report.
Conversely, the report concludes, despite noting the difficulties in finding comparable data across countries: “Although no single behavior can explain the U.S. health disadvantage, the high prevalence of multiple unhealthy behaviors in the United States may play a large role.” The debate is between those who would attribute those behaviors to a lack of “personal responsibility” versus those who would blame social and economic factors. The authors lean toward the idea that there may be a relationship between worsening in comparable social conditions in the U.S. — income inequality, poverty, child poverty, single-parent households, divorce and incarceration — and the health gap with other countries.
Also, the authors suggest that differences in the built environment in the U.S. — human settlement patterns, as we like to say on Bacon’s Rebellion — contribute to the American health disadvantage. “It is plausible to hypothesize that factors in the built environment related to low-density land development and high reliance on automobile transportation; environmental factors related to the wide availability, distribution, and marketing of unhealthy foods; and residential segregation by income and race … may be important contributors to the U.S. health disadvantage in many domains.”
Bacon’s bottom line: Only one conclusion seems indisputable from this report: Understanding the causes of the health gap between the U.S. and other developed countries is incredibly difficulty and fraught with methodological issues. All conclusions seem tentative and subject to additional research. However, that said, it seems clear, though perhaps not indisputable, that the health gap can be attributable only in part, if at all, to differences between the U.S. and other health care systems. (The high cost of the U.S. health care system is a different issue, which this study did not address.)
Any intelligent discussion of public health needs to consider differences in socio-economic conditions, social values, individual behaviors and the built environment. I come away from this report feeling vindicated about Bacon’s Rebellion‘s editorial emphasis on walkable/bikable communities, food deserts/locally grown food, and clean water. If we want to improve community health, those are very good places to start.



